![Molécule]()
Serotonin implicated in migraine
Serotonin and migraine
Various studies have implicated serotonin in migraine. Serotonin constricts nerve endings and blood vessels and thus affects pain. The team of Comings in the USA, postulated that
a low level of serotonin causes dilation of the vessels and
participates in the triggering of migraine . Migraineurs often report that their
headaches stop after vomiting . Vomiting stimulates intestinal motility and
increases serotonin levels in the blood. Previously, it was suggested that fluctuations in serotonin levels likely lead to pH shifts in the brain, thereby causing migraine, since serotonin, also known as 5-hydroxytryptamine (5-HT), is a
basic amine. In the brain, normal levels of
erotonin (5-HT)
prevent migraines . This finding has been made in
migraine without aura but also in
migraine with aura ,
ophthalmic migraine and
vestibular migraine .
The lack of serotonin would leave powerful vasodilators (like nitric oxide) unopposed. This is why we observe during migraines a dilation of the blood vessels on MRIs.
Lack of serotonin influences migraine
The vessels of the brain respond to serotonin by vasoconstriction , that is, they contract. However, in migraine, there is a vasodilation of the blood vessels. This is mainly induced by 2 substances. On the one hand, nitric oxide (NO) which is found massively during the migraine attack and on the other hand CGRP , a peptide which promotes the dilation and inflammation of the vessels. Moreover, new treatments such as CGRP antibodies have been developed to relieve chronic migraines. Studies have shown that serotonin agonists, that is to say molecules that will behave like this one, promote the reduction of migraine attacks as well as the intensity of pain. One might suggest that the release of serotonin during migraine has two purposes. Act on vasodilators by lowering the level of (CGRP) and opposing the effect of nitric oxide.
Tryptophan as a dietary supplement
Serotonin comes from an essential amino acid which is L- Tryptophan . Essential means that it is not metabolized by the body but needs to be provided by food. From tryptophan the body synthesizes serotonin. If the migraine patient has a deficiency or lack of serotonin, one of the solutions is to provide him with a tryptophan supplement to promote the production of the molecule. Several studies have shown that L-Tryptophan in a dietary supplement can gradually reduce migraine attacks .
The role of serotonin in migraine
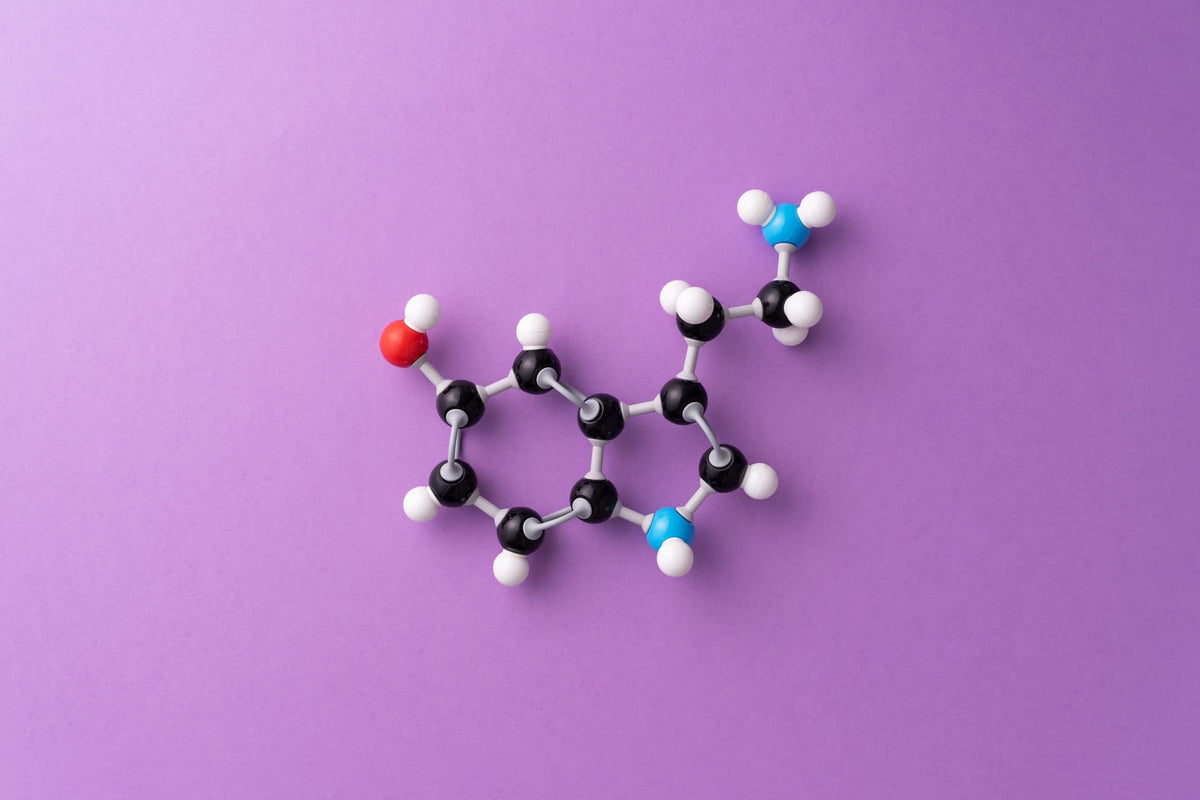
Serotonin or
5-hydroxytryptamine (5-HT) is a neurotransmitter essentially synthesized in the brain from an amino acid, L-tryptophan. After being released by serotonergic neurons, serotonin is reuptaken by 5-HTT (or SERT) transporters or broken down to 5-hydroxyindole acetic acid (5-HIAA), which can be measured in blood, urine or brain fluid. -spinal. The serotonergic system is involved in regulating the
sleep/wake cycle , maintaining
alertness ,
concentration ,
mood , and
pain (David et al. 2016). Sicuteri's observation in 1961 of an increase in the urinary excretion of 5-HIAA in migraine patients was the starting point of interest in serotonin in migraine (Sicuteri 1961). During a
migraine attack , a 30% increase in the level of 5-HIAA is found in the patient's cerebrospinal fluid on average, showing a significant production of serotonin (Bousser et al. 1986; Ferrari et al. 1993). The origin of serotonin during an attack could come from blood platelets (Fozard et al. 1994), but also from perivascular fibers (Launay et al. 2003). It is interesting to note that the start of
treatment with antidepressants tends to induce
headaches in migraine patients . The hypothesis is that
antidepressants lead to a transient increase in free (extracellular) serotonin levels which would cause headaches, before observing
the protective effect of serotonin in depressed patients (Azimova et al. 2016; Xu et al. 2017). This hypothesis was confirmed by a study on reserpine (Lance et al. 1991), a molecule capable of massively releasing serotonin from platelets. This induces
headaches in migraine sufferers , but not in healthy subjects after its injection.
Thus migraine patients could suffer from a chronic deficit of serotonin and the crisis would be the consequence of a sudden increase in its rate .
In addition, a significant increase in 5-HTT transporters responsible for recapturing serotonin (Nagy-Grócz et al. 2017) has been shown in the brainstem in migraine patients, implying serotonergic dysregulation. If the serotonin level is naturally low in the migraine patient, this could be the consequence of chronic L-tryptophan depletion; this is the finding of Ren's team (Ren et al. 2018) which records low levels of this amino acid in migraine patients. Finally, could this set of deregulations found in these patients not be the expression of a much more global metabolic disorder?
Azimova, JE, KV Skorobogatykh, AV Sergeev, and EA Klimov. 2016. “Migraine and depression: efficacy and safety of antidepressant therapy”. Zhurnal Nevrologii I Psikhiatrii Imeni SS Korsakova 116 (11): 35‑40. https://doi.org/10.17116/jnevro201611611135-40. Bousser, MG, JL Elghozi, D. Laude, and T. Soisson. 1986. "Urinary 5-HIAA in Migraine: Evidence of Lowered Excretion in Young Adult Females." Cephalalgia: An International Journal of Headache 6 (4): 205‑9. https://doi.org/10.1046/j.1468-2982.1986.0604205.x. David, DJ, and AM Gardier. 2016. “The pharmacological basis of the serotonin system: Application to antidepressant response”. The Brain 42 (3): 255‑63. https://doi.org/10.1016/j.encep.2016.03.012. Ferrari, Michel D, and Pramod R Saxena. 1993. "On Serotonin and Migraine: A Clinical and Pharmacological Review." Cephalalgia 13(3): 151-65. https://doi.org/10.1046/j.1468-2982.1993.1303151.x. Lance, JW 1991. “5-Hydroxytryptamine and Its Role in Migraine”. European Neurology 31 (5): 279-81. https://doi.org/10.1159/000116754. Nagy-Grócz, Gábor, Zsuzsanna Bohár, Annamária Fejes-Szabó, Klaudia Flóra Laborc, Eleonóra Spekker, Lilla Tar, László Vécsei, and Árpád Párdutz. 2017. “Nitroglycerin Increases Serotonin Transporter Expression in Rat Spinal Cord but Anandamide Modulated This Effect”. Journal of Chemical Neuroanatomy 85 (November): 13‑20. https://doi.org/10.1016/j.jchemneu.2017.06.002. Ren, Caixia, Jia Liu, Juntuo Zhou, Hui Liang, Yayun Wang, Yinping Sun, Bin Ma, and Yuxin Yin. 2018. “Low Levels of Serum Serotonin and Amino Acids Identified in Migraine Patients.” Biochemical and Biophysical Research Communications 496 (2): 267-73. https://doi.org/10.1016/j.bbrc.2017.11.203. Sicuteri, F. 1961. “Introduction of serotonin antagonists in therapy”. La Clinica Terapeutica 21 (October): 394-423. Xu, Xiao-min, Yang Liu, Mei-xue Dong, De-zhi Zou, and You-dong Wei. 2017. “Tricyclic Antidepressants for Preventing Migraine in Adults”: Medicine 96 (22): e6989. https://doi.org/10.1097/MD.0000000000006989.